OCD or Eating Disorders
What we can improve
There are several similarities between obsessive-compulsive disorder (OCD) and eating disorders such as anorexia or bulimia nervosa. For both of these issues, there are obsessive thoughts and / or compulsive behaviors, and anxiety is also often present.
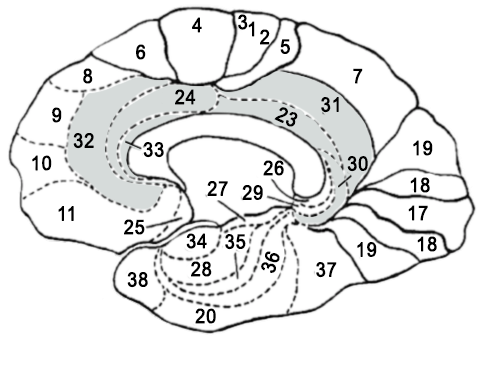
After analyzing over 87,000 SPECT Scans, the renowned American psychiatrist Dr. Daniel Amen explains in his trainings, the brain profiles often associated with OCD, as well as with eating disorder. First, prefrontal lobes play an important role in judgment. Normally, they are supposed to be able to influence the process of reasoning so that the person realizes that their behavior is inappropriate. For example, if a person plays poker at the casino and bets a disproportionate amount, the prefrontal lobes should be able to suggest to the individual not to take that risk.
A second brain region that plays a role in OCD and eating disorders is the cingulate gyrus. This region plays a role in mental flexibility. Dr. Amen presents in his studies that a hyperactive cingulate gyrus brings mental rigidity. In such cases, when a person has a fixation on something, it will be difficult for them to “get out” of that thought, whether it be food, thought, or behavior.
Finally, as there is often anxiety in individuals with these problems, when we perform the quantitative electroencephalogram (qEEG), the neuropsychologist will pay particular attention to the amygdala and other areas involved in anxiety. If he notices significant deviations in the activity of these regions (often hyperactivity), we will then want to train them, using with Neurofeedback. You can go to the page on anxiety for more information.
In cases of OCD or eating disorders, we will often want to train the prefrontal lobes, the cingulate gyrus as well as the anxiety network (which includes the amygdala). Studies have shown that Neurofeedback trainings can bring significant improvements in these behaviors.
Prefrontal Lobes
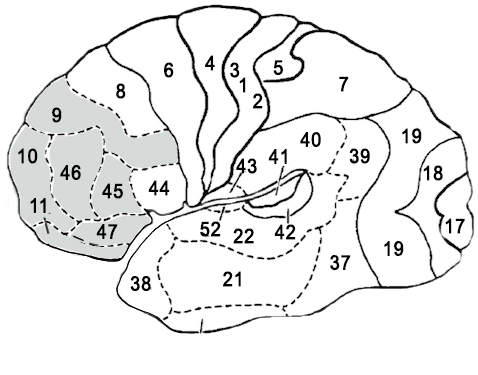
Cingulate Gyrus
- Less in unwanted behaviors
- Better mental flexibility
- Improved judgement
- Decreased anxiety
- Increased feeling of well-being
In the case of OCD, a 2003 study by Hammond1 shows that Neurofeedback training resulted in an 89% reduction in OCD symptoms according to a recognized measure from Padua Inventory. A follow-up that was carried out 12 months after the training shows that the improvements have been maintained and that the behaviors have not returned.
For eating disorders, a scientific article published in 2018 in the journal Nutrient2 reviews the studies conducted to date. In this one, we mention that, according to two controlled studies, the individuals having carried out 10 sessions of Neurofeedback showed a decrease in the number of episodes of distress and overconsumption of food. In addition, a follow-up conducted three months after the end of training showed that the improvements were maintained.
The article also describes 4 other studies that have demonstrated a decrease in undesirable behavior related to eating disorders as well as an improvement in health following Neurofeedback trainings.
1. Hammond, D. C. (2003). QEEG-guided Neurofeedback in the treatment of obsessive compulsive disorder. Journal of Neurotherapy, 7(2), 25-52.
See Article
2. Feedback-Based Treatments for Eating Disorders and Related Symptoms: A Systematic Review of the Literature
Nutrients, 2018
See Article
Le trouble du déficit de l’attention avec ou sans hyperactivité (TDA/TDAH) est une condition neurodéveloppementale complexe qui toucherait 5 à 8 % des enfants. Il peut être décrit par une panoplie de symptômes liés à des dysfonctions ou à une pauvre maturation des lobes frontaux.

Eating disorders have serious consequences on physical and mental health. They can manifest at a young age and affect the personal and professional lives of affected individuals. There are different types of eating disorders, each with specific symptoms.
Anorexia Nervosa
This obsessive-compulsive disorder (OCD) mainly affects women. Anorexia nervosa is characterized by food restriction aimed at significant weight loss, and an intense fear of becoming fat despite being thin. Anorexia nervosa is also characterized by an alteration of body image and weight perception.
If you have anorexia nervosa, you may feel like you’re eating too much and sometimes deprive yourself of food for fear of gaining weight. In the same vein, you may consume slimming pills and laxatives. You may also experience unexplained weight loss, and your body may show signs of deficiency (hair loss, yellowing of the palms, absence of menstruation, etc.). You also experience moments of anxiety, depression, and irritability. You have difficulty concentrating and engaging in physical activities excessively.
If you notice symptoms of anorexia in a family member or yourself, seek professional help.
Avoidant/Restrictive Food Intake Disorder
This condition leads to difficulties in eating reasonable amounts. A person with Avoidant/Restrictive Food Intake Disorder may experience:
appetite disturbances,
sensory sensitivity making eating difficult,
general disinterest in food,
past negative experiences leading to eating difficulties,
loss of energy, endurance, and growth,
and lack of concentration.
Patients with this disorder struggle to consume enough calories and nutrients.
Binge Eating Disorder
Presented as regular and uncontrollable binge eating episodes, binge eating disorder differs from bulimia in the absence of compensatory behaviors. In the case of a binge eating disorder, you may tend to eat large amounts of food without feeling hungry. You may also experience abdominal distension, depression, or even overweight or obesity. Joint pain and cardiac fatigue may also occur.
Implementing a diet is useless in treating this eating disorder, whether in young patients or adults.
Bulimia
Bulimia manifests as abnormal ingestion of food volume in a limited time, compulsively or ritualistically. Patients generally presenting this OCD are impulsive and emotional individuals. More common than anorexia nervosa, bulimia has the following symptoms:
abuse of fasting or physical exercise,
use of laxatives or diuretics to neutralize weight gain,
yellow teeth, swollen cheeks and jaws due to regular vomiting,
loss of energy,
constipation,
heart problems,
esophageal inflammation.
A person with bulimia may have a “normal weight”, which can contribute to concealing the eating disorder from others. Like anorexia nervosa, this OCD is, however, a serious medical condition that requires professional treatment.
Pica
A feeding disorder that lasts for at least one month, pica is characterized by an uncontrollable need to consume non-nutritive substances such as earth, paper, or even soap. Repeated ingestion of non-food products can alter the patient’s normal development. Pica manifests with several symptoms, such as vomiting, constipation, abdominal pain, anemia, growth retardation, or even lead poisoning.
A person with pica may have a coexisting intellectual disability or another mental disorder, such as autism.
Rumination Disorder
This rare feeding disorder affects infants, children, and adults. People with rumination disorder involuntarily regurgitate food they have previously swallowed, chew it again, and then swallow it or spit it out. The regurgitation occurs daily for at least one month and usually follows a meal.
Patients with rumination disorder are not nauseous before regurgitation, which is not related to a gastrointestinal disorder. This eating disorder can cause weight loss, bad breath, dental problems, and physical complications if not treated.
Eating disorders are multifactorial and can arise from a combination of genetic, biological, behavioral, psychological, and social factors. Seek professional help if you suspect you or someone you know has an eating disorder.
L’évaluation diagnostic de TDAH
Le diagnostic de TDAH n’est pas simple à poser et il n’y a aucun examen médical qui permet de le faire de manière précise. Le professionnel de la santé, notamment le neuropsychologe, qui pose le diagnostic de TDAH fait une évaluation complète de l’enfant et de son milieu de vie. Ce spécialiste peut s’intéresser à plusieurs éléments :
- le développement de l’enfant depuis sa naissance,
- son comportement à la maison, à l’école et ailleurs,
- ses symptômes (intensité et durée),
- ses difficultés à l’école ou lors de l’exécution des tâches.
Pour pouvoir déterminer si un enfant souffre d’un TDA ou TDAH, le neuropsychologue ou autre professionnel habileté à faire le diagnostic, peut utiliser les critères comportementaux élaborés par l’ouvrage Manuel diagnostique et statistique des troubles mentaux, 5e édition ainsi que des des outils psychométriques. Les tests psychologiques et les tests neuropsychologiques peuvent également aider à poser un diagnostic de TDAH.
À noter : L’électroencéphalogramme permet de préciser les profils d’activité électriques dans le cerveau pouvant apporter des problèmes au niveau des fonctions exécutives (concentration, attention, planification, organisation, impulsivité et agitation mentale ou physique). Toutefois, l’EEGq ne permet en aucun cas de poser le diagnostic de TDA ou de TDAH
Lorsqu’un enfant présente des troubles de l’attention ou de la concentration, cela peut être dû à un fonctionnement non-optimal de certaines régions du cerveau. Grâce au neurofeedback, on peut réduire progressivement les symptômes du TDA ou TDAH. Il est basé sur un traitement par conditionnement opérant permettant au cerveau d’identifier les fonctionnements électriques optimaux et de les corriger.
Le neurofeedback permet à votre cerveau de retrouver un fonctionnement optimal et ’améliorer vos comportements et compétences dans votre vie quotidienne. Neuroperforma dispose d’un équipement de dernière génération pour réduire les symptomes du trouble du déficit de l’attention avec ou sans hyperactivité. Votre professionnels vous proposera des séances régulières pour des résultats durables.
La prise de médicaments (psychostimulants) peut être nécessaire pour réduire les symptômes.
Il existe aussi d’autres méthodes naturelles comme la méditation et l’apprentissage de stratégies de travail et d’organisation efficaces. On peut citer le livre Mon cerveau a besoin de lunette (version pour enfants et version pour adulte).
La différence entre les deux, c’est que le TDA est une condition impliquant seulement des difficultés d’attention sans présence d’hyperactivité physique et mentale. En revanche, le TDAH est un trouble du déficit de l’attention avec hyperactivité. Les enfants souffrant de TDAH sont généralement perçus comme des personnes qui débordent d’énergie, qui ont la bougeotte et qui sont intenses ou impulsifs.
À la maison, les enfants atteints de TDAH font souvent des crises de colère. Ce qui crée des tensions importantes au sein de la famille. Les enfants TDA quant à eu sont souvent lunatique et ont de la difficulté à se mettre à la tâche. La période des devoirs peut être compliquée entre l’enfant et ses parents. À l’école, les enfants manifestant un TDA ou un TDAH présentent un risque d’avoir des difficultés d’apprentissage en lecture et pour accomplir les tâches. Ils peuvent se retrouver en situation d’échec s’ils ne sont pas rapidement pris en charge. Le TDAH affecte donc négativement la vie scolaire, sociale et familiale de celui qui en souffre.
Les enfants issus de familles présentant ce trouble sont susceptibles de développer les symptômes y afférant.
Lorem ipsum dolor sit amet, consectetur adipisicing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Nulla consectetur mauris ante, id aliquet ligula vehicula vel aliquam vitae orci et justo suscipit. Veniam quis nostrud exercitation ullamco laboris aliquip ex ea duis aute irure dolor kin reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur excepteur sint occaecat.


